Review Article
Responding to Disasters: More than economic and infrastructure interventions

David Crompton OAM1*, Ross Young2, Jane Shakespeare-Finch3 and Beverley Raphael AM4
1Professor, Metro South Addiction and Mental Health Services, Australian Institute Suicide Research and Prevention, Griffith University, Queensland University of Technology, Australia2Professor, Faculty of Health Queensland University of Technology, Australia
3Professor, Faculty of Health Queensland University of Technology, Australia
4Professor, Australian National University Medical School, Australia
*Address for Correspondence: Professor, David Crompton OAM, Metro South Addiction and Mental Health Services, Australian Institute Suicide Research and Prevention, Griffith University, Queensland University of Technology, Australia, Tel: +61731569806; Email: [email protected]
Dates: Submitted: 31 March 2018; Approved: 23 April 2018; Published: 24 April 2018
How to cite this article: David Crompton OAM*, Young R, Finch JS, Beverley Raphael AM. Responding to Disasters: More than economic and infrastructure interventionsntions. Insights Depress Anxiety. 2018; 2: 014-028. DOI: 10.29328/journal.ida.1001007
Copyright License: © 2018 David Crompton OAM, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Objectives: Natural disasters confront individuals, communities and governments with the challenge of rebuilding and addressing psychosocial sequelae. With the increasing number of natural disasters it is timely to evaluate the efficacy of interventions and strategies to address the mental health needs of individuals and the community.
Method: An evaluation of literature related to the psychological impact of natural disasters, treatment efficacy and government strategies to confront the social and psychological impact of natural disasters for the period 1983-2016 was undertaken.
Results: Epidemiological studies following natural disasters despite the use of differing psychological measures demonstrate significant psychological morbidity - anxiety (7-42%), complicated grief (28-41%), depression (6.5-38%), post-traumatic stress disorder (11-89%) and substance misuse (1.3-24%). Intervention studies post-disaster demonstrate efficacy variability.
Conclusions: The increase in the number and impact of meteorological and hydrological events since the 1980s and the psychological, social and economic consequences of these events has resulted in the development and implementation of government policies to confront the immediate and long-term adverse outcomes. The focus is typically on resources and infrastructure redevelopment with less focus on social and mental health interventions with long-term evaluation of interventions uncommon. The consequence of natural disasters emphasizes the importance developing strategies to ensure effective evaluated psychosocial interventions are available across at-risk communities.
Introduction
The capacity to respond to a disaster is influenced by the event and the social, economic, cultural and political consequences that impact on the community, organizations and individuals. Recognition of the importance of a collaborative whole-of-government approach to disasters is emphasized by Australian and State Government Disaster management strategies that accept a collective approach that encompasses community sector, emergency services, defense forces, government agencies, business and individuals. A significant aspect of this planning is the identification of the need to enhance national and individual resilience through risk management that engages the individual, government and other agencies in planning, preparation and implementation of all hazard prevention strategies that use and build on individual and community capacity. The development of a strategy to provide high-level guidance on disaster management across all levels of government, not for profit organizations, community and business leaders and families and individuals was perceived as a crucial initial step to enhance Australia’s capacity to provide a sustainable response to the many natural disasters that impact on the country [1,2]. The strategy focuses on risk mapping, the built environment and training of volunteers and emergency workers.
The national approach while identifying the role of mental health as integral to recovery [3,4] highlights that the mental health response is not just about building resilience but also addressing the mental health impact on the community, families and individuals. Identification of the dynamic and variable nature of the effect of disaster is evident with short and long-term adverse outcomes and positive outcomes from disasters [4,5].
Despite recognition of the need for a planned, coherent, inclusive and resourced approach to mental health care there remains variability across jurisdictions and countries with respect to each of these facets. The consequent gaps in clinical services and the unmet mental health needs across communities is associated with an increased likelihood of negative social, economic and health outcomes for individuals affected by mental illness [6]. These gaps in planning and resource development are accentuated during natural and man-made disasters [7]. Irrespective of the cause of a disaster, epidemiological data indicate individuals and communities may experience adverse mental health, social and economic consequences [8-10].
The adverse outcomes of exposure to trauma, although argued by some as a phenomena of the post-Vietnam era [11] is documented in historical literature and scientific publications. As early as 1756 a case study described individuals who developed sleep disturbance, difficulties returning to work and emotional lability after being trapped in a snow avalanche [12-14].
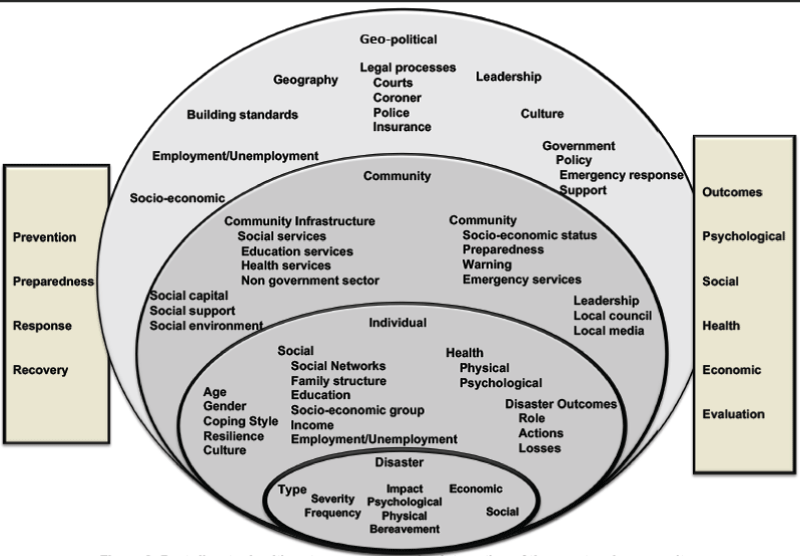
The emotional, behavioral and social responses following exposure to a natural disaster range from severe anxiety and grief to mild or minimal emotional distress. The survivors of the 1999 Turkey and 2008 Wenchuan earthquakes, 2004 Tsunami, and Hurricane Katrina experienced significant psychological morbidity. Evaluation of the psychological impact of disasters and effectiveness of interventions (Table 1) delivered to affected communities is however, compromised by the variability of psychological measures used to assess those exposed to disasters. The use of instruments that combine depression and PTSD in a single measure (Traumatic Stress Symptom Checklist (TSSC)-17 DSM-IV PTSD and six depression symptoms) [15] or only rate psychological distress (BSRS-5) [16] create complexities with respect to evaluation of symptom severity and the many factors that may influence the development of psychological symptoms and the efficacy of interventions. Variability in the rate of mental disorders after disasters is apparent from studies that identify the prevalence of PTSD ranging from 8.3-89%, depression 8-35% and anxiety 7-43%. Several studies have found factors such as age, proximity to the event, disaster severity and bereavement influence the likelihood of developing symptoms and the severity of psychological sequelae [17-19].
Studies consistently demonstrate social supports; ongoing stressors and relocation affect the likelihood of developing PTSD, depression, anxiety and alcohol or substance misuse [20,21]. The complex relationship between disaster exposure and psychological sequelae is highlighted by the risk of developing alcohol dependence or misuse. A two-year follow-up of a population impacted by 9/11 identified that delayed onset PTSD was associated with an increased rate of alcohol misuse [22], while a study of 899 Norwegians who resided in an area affected by the 2004 Tsunami demonstrated variability in alcohol misuse and an absence of a relationship between current alcohol use and disaster exposure. The consumption of alcohol in this population found a bivariate relationship between severity of PTSD symptoms and the perception of increased or decreased alcohol [23]. Following Hurricanes Katrina and Rita a prospective study found alcohol misuse was more likely to occur in individuals with a previous history of trauma and low income [24]. Although a systematic review found 22% used alcohol as a coping strategy, the rate of alcohol abuse in survivors was only 0.3% [25].
The suicide rate following natural disasters also highlights the variability in the psychosocial outcomes. A study following 1999 Taiwan earthquake found the affected population had 1.46 times increased risk of committing suicide. Pre-existing mental illness and living in a rural environment predicted the increased risk of suicide in this study [26]. Following the 2011 Fukushima earthquake and tsunami there was a reduction in the standardized suicide mortality rate (SSMR) but by 2014 the rate exceeded the pre-event SSMR. This occurred on the background of social, family and community disruption and elevated rates of mental health illness [27]. Although post-disaster systematic reviews have found increased suicide rates, this increase was accounted for by factors such as the presence of pre-event mental illness [28]. In contrast, a review of post-disaster suicides in the United States (1982-1989) found no difference in the suicide rate for events such as floods, tornadoes, storms or earthquakes [29]. The difficulty in understanding this variability in suicide rates reflects, not only the presence of pre-event factors but also the reduction in risk factors for suicide, as identified in the 1997 Red River flood study [30].
The impact of natural disasters is not limited to adverse psychological outcomes. An increase in interpersonal violence occurred post-Hurricane Katrina [31]. Following Hurricane Andrew there was an increased rate of foetal distress and an adverse impact on female reproductive health [32]. A systematic review of births and reproductive health following disasters found variability with respect to the methodology and focus of each study. This review however reinforced that disasters may adversely impact on reproductive fertility and birth outcomes [33].
Vulnerability to the destructive consequences of natural disasters is nevertheless not just a function of individual dynamics, but is linked to social and economic parameters. An OECD evaluation that included data from New Zealand, Japan, Turkey, Australia and the United States found displacement and relocation of people, unemployment, loss of income and disruption of businesses disproportionately increased vulnerability to disasters [34]. This study also found the young, and female more likely to experience adverse outcomes. In developing countries, vulnerability to disasters, socioeconomic inequality and an inability to effectively respond to events, accentuates elements identified in the OECD report. The health, social and economic inequalities in developing countries further amplify the deleterious outcomes of natural disasters [35].
In addition to age and gender other studies found that frequency, type and magnitude of the disaster and accumulated stressors influence the likelihood of developing emotional and behavioral responses following mass trauma and disasters. These factors and the expansion of urban communities with their associated economic, social, infrastructure and environmental vulnerability can further complicate the disaster response [24,36-39].
Confronting the various elements that influence disaster recovery requires planning to address multiple community expectations, including infrastructure redevelopment, health, and social care interventions. These aspects of disaster management occur across multiple systems and timeframes. The necessity for short and intermediate term interventions is highlighted in a number of studies [39] [40]; however recovery may take from months to years. Pre-existing mental illness, access and capacity to engage with mental health services, social factors, grief, individual and community coping strategies and resilience influence the recovery journey and, potentially exacerbate the adverse economic and social outcomes for individuals and affected communities [41-44].
Response to a natural disaster requires a broad social, psychological and economic plan that is systematic, effective and inclusive of social and psychological responses [45], while embracing a broad community engagement [46]. Recovery from a disaster does not end when infrastructure is rebuilt or when families return to their home. It is an ongoing process that encompasses the emotions that surround the rebuilding of homes, families and the community, aspects that may not have a clear end point [47].
Mental health interventions after a disaster
Although there are a wide range of evidenced-based individual and group therapies interventions that assist recovery from emotional distress and psychiatric disorders [48-51], the provision of services to those experiencing distress following a disaster is challenged by the imperatives of re-establishing accommodation, reconnection of essential utilities and reconstruction of the community and workplaces. The provision of psychological and social supports post-disaster were identified by Jacobs (1995) [52] as key strategies that facilitated the adoption of coping strategies to assist survivors and responders and community adaptation and recovery. Experience gained from multiple disasters affirms the need to implement integrated individual and community support that is inclusive of government, disaster relief agencies and organizations and specialist mental and public health services. The structured and integrated disaster plans should be inclusive of the community input.
The development of disaster plans has resulted in the inclusion of early intervention programs such as Psychological First Aid (PFA). Demonstration of the benefits of PFA remains difficult [53-56]. Several studies have demonstrated the positive effect of psychological interventions for those affected by natural disasters (Table 1). There is however, variability in the type and duration of interventions, and the number of survivors evaluated in these studies. The variation in therapies, treatment duration and the assessments used confound post-disaster outcome research. The inconsistency with respect to intervention types and duration is highlighted by two adolescent studies. One study used group and individual trauma or grief focused therapy in 36 participants [57] with the second a manual based three-day CBT program [58]. The modified behavior therapy treatment program used after a Turkish earthquake, while demonstrating efficacy provided outcome data for only 75 of the 231 who entered the study [59]. In contrast, the Victorian bushfires intervention study used data from 261 people. There was despite a focus on CBT, variability in intervention types [60] with the number offered treatment small in comparison to the number affected.
Although there is variation in methodology and treatment type, evidence does support the necessity to establish programs that recognize those who have developed mental health problems [61,62] and provide evidence-informed treatment across the community. These programs should be accessible, support local health care providers, have the capacity to be delivered face-to-face and through other technologies and address the unmet mental health needs of individuals affected by disasters [43].
Government and community response to disaster
Disasters place significant demands on community resources, require collaboration and the need to undertake at times, unfamiliar tasks. The bringing together of emergency and public and mental health services [63,64] can be assigned a lower priority when compared to infrastructure repair and food safety. The disaster response often overlooks the enduring cost to the community of adverse mental health outcomes that occur following a natural disaster [65].
To overcome the deleterious mental health consequences of disasters there is a need to support interventions that address, the social, emotional and mental health functioning of the community [41,66,67]. Interventions require a whole-of-government collaboration that connects with the community and engages with affected individuals, and is inclusive of non-government agencies and the private sector [68]. Timeliness, effectiveness, resource capacity and capability affect the psychosocial response to a disaster, and the effectiveness and extent of individual and community recovery [69,70]. Disconnection between the devastation of a disaster and the extent and effectiveness of the all-hazard response is highlighted by the response to Hurricane Katrina. Evaluations after the hurricane identified gaps in evacuation procedures, environmental health interventions and emergency and mental health responses. The ferocity of the hurricane, resource availability, geography, social, cultural and economic vulnerability accentuated the impact of Hurricane Katrina and the challenges confronting the response of government and non-government agencies [71,72].
The Victorian Black Saturday Fires of 2009, and the study of Texan floods between 1997-2001 [32,73-75] emphasize the multiple components that challenge disaster planning and management and sway disaster outcomes. Natural disasters usually do not occur in isolation, with Australian bushfires often occurring on the background of long-term droughts that are associated with significant psychosocial distress [76]. The association between pre-disaster factors and adverse outcomes was identified in a study of Texan floods that found social vulnerability increased casualty rates. This study also found that all-hazard planning must consider the consequence of disaster mitigation strategies. Although flood mitigation reduced casualties in some areas, the misleading sense of safety in other areas, promoted a misplaced sense of security and consequently increased casualties in ‘safe areas’. These multiple and variable pre and post disaster factors impact on individual and community recovery and resilience [32,73].
The requirement for an integrated response to address the complex problems induced by disasters has resulted in the development of cohesive response models. The systematic response to the floods and cyclones that occurred in Queensland, Australia between December 2010 and February 2011 reflect the integrated Government and Non-Government sector response that occurs in the Australian setting. This approach is inclusive of pre-disaster planning and immediate to long-term disaster management. The disaster management plan includes the emergency response, safety of infrastructure, reconstruction and social, psychological and health interventions [77-79].
The floods and cyclones during this period affected 68 of Queensland’s 73 Local Government Authorities (LGAs). Over 1.3 million people were affected by the disaster. Based on international data, estimates indicated up to 314,000 were vulnerable to emotional distress with a one percent in severe mental disorders and a five percent increase in mild to moderate mental disorders [80]. During the crisis, 10,500 people were evacuated from their homes, cities and towns became totally isolated, and 250 patients required aero-evacuation from the Cairns public and private hospitals to Brisbane Hospitals; a distance of 1400Km [81].
The immediate response to the disaster ranged from involvement of the Police, State Emergency Services, Red Cross [82] and military [83] to the implementation of the Reconstruction Authority. The Authority focused on six medium to long-term initiatives; Human and Social, Economic, Environment, Building Recovery, Roads and Transport and Community Liaison and Communication [84]. Given the identified risk of adverse psychological outcomes the recovery program supported the implementation of a mental health program for individuals and communities. The Queensland Mental Health Natural Disaster Recovery Plan 2011–13 (The Plan) adopted a public health model that sought to address the psychosocial impact of the floods and cyclones on communities, schools, families and individuals through a collaborative approach linking primary health care, schools, non-government sector, community-based support, and specialized mental health services that offered the capacity to provide services to at-risk populations such as the bereaved, affected communities and areas where the provision of trauma informed services were usually unavailable or difficult to access. The Plan was based on the WHO [80] population models for psychological morbidity following a disaster and built on the psychological first aid program initially provided across communities [66], with local community initiatives that promoted community connectedness, web-based programs and information dissemination.
The Centre for Trauma, Loss and Disaster Recovery funded through the Commonwealth and State Government Natural Disaster Relief and Recovery Arrangements (NDRRA) was formed to oversight the implementation and management of The Plan that was required to address the needs of vulnerable populations, provide evidence-informed treatment programs and enhance resilience within affected communities and individuals [79,85]. The Plan required the establishment of a statewide Skills for Psychological Recovery (SPR) training program to enhance access to skilled local primary care clinicians [86], a 24 hour access line and specialist disaster mental health teams for children and adolescents [87] and, adults (18+) with the access and treatment services utilizing standardized assessment and evidence-informed treatment programs. In recognition of the complex psychosocial and legal needs of those who lost family members due to the floods and cyclones a Bereavement Team was initiated [20,88]. Although the response to the Floods and Cyclones of 2010/11 was described as ‘global best practice’ the paper did not address the importance of responding to mental health issues in the aftermath of disaster. The focus during the crisis was perceived as restoration of normalcy [81] an outcome that is challenged by the death of family members, loss of properties, personal items such as family photos and the need to confront the problems of rebuilding, relocation, legal settlements and commissions of enquiries. This separation of the psychosocial response from the structural and emotional devastation that may occur after a natural disaster challenges the recovery of individuals and communities.
Meeting the challenge of natural disasters
A countries capacity to provide effective psychosocial interventions that are key factors in relation to reducing the short and long-term mental health sequelae of disasters [89] is linked to mental and health care planning which is influenced by government models of mental care that range from the inclusiveness of Canadian and United Kingdom’s models to the fragmented model that occurs across the United States. This planning is confronted by the disproportionate increase in the number and impact of meteorological (cyclones, hurricanes) and hydrological (floods) events since the 1980s [90].
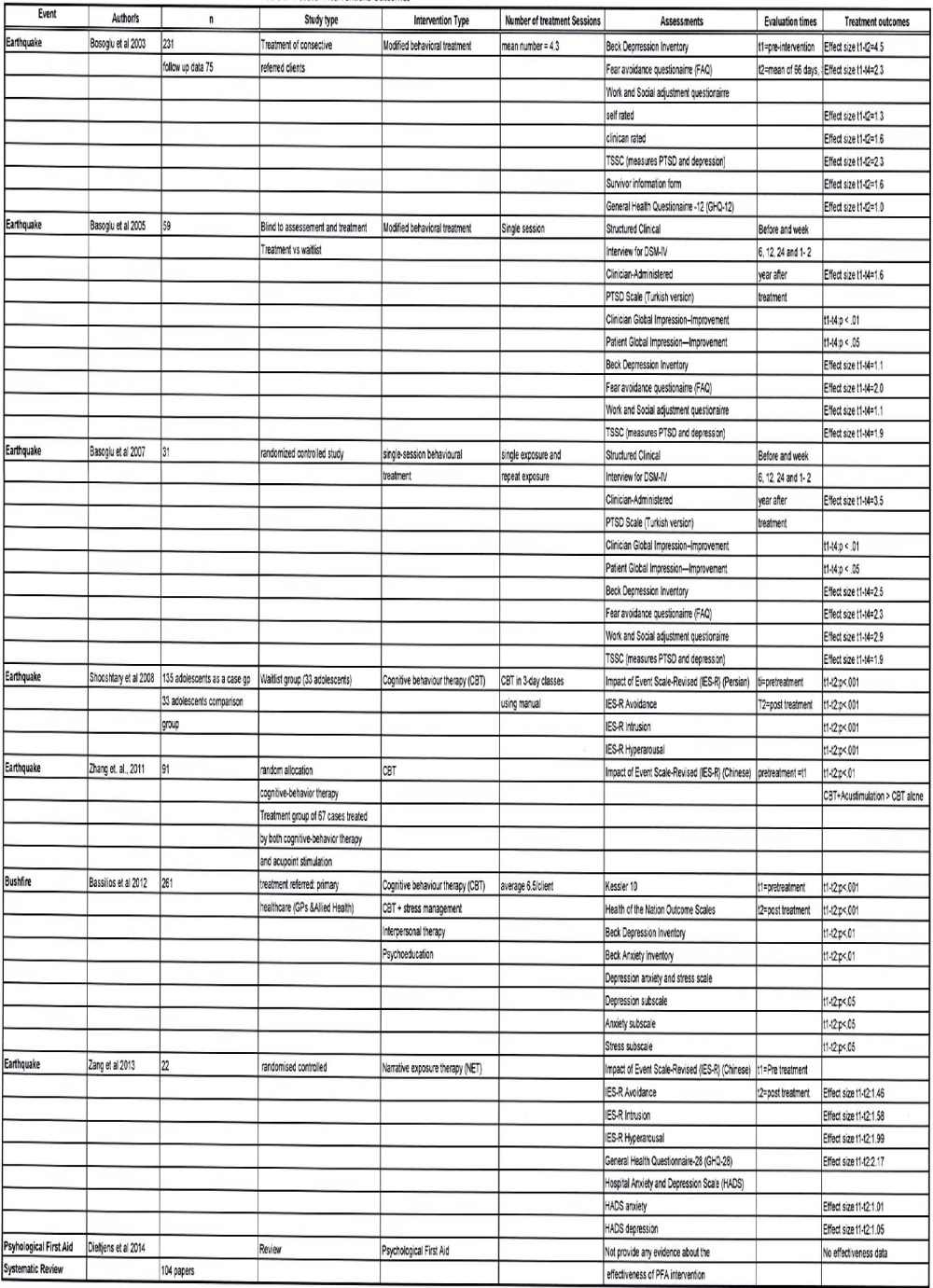
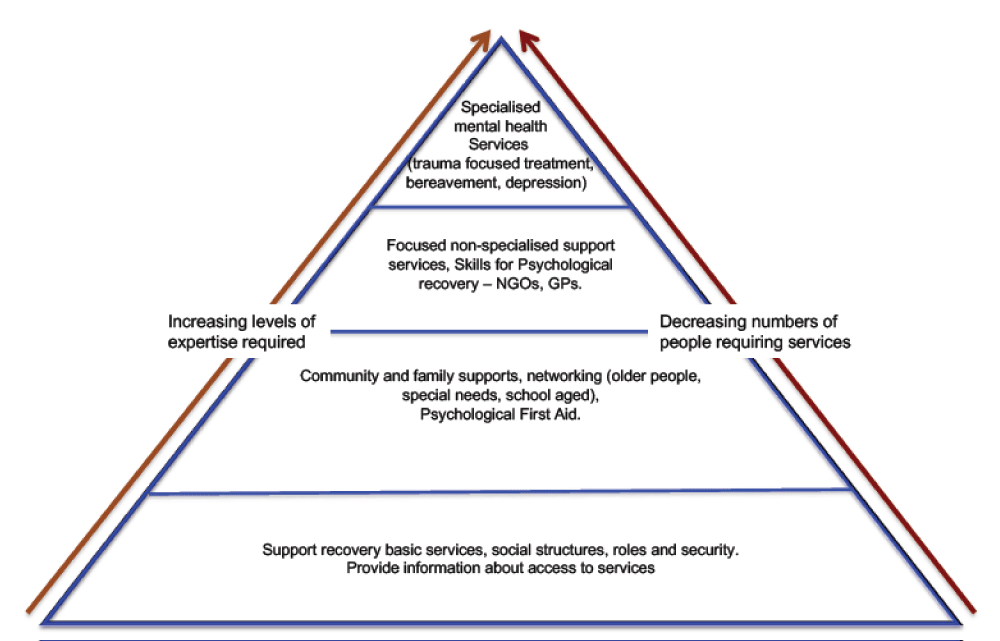
The increase in natural disasters confronts governments of developed and developing nations. The current response models demonstrate gaps in relation to the capacity to meet the mental health and social care needs of communities, identification of those at-risk and provision of evidence-informed care to impacted communities, families and individuals. These response models (Figures 1 and 2) [41,91,92] have resulted in a restricted vision of disaster planning and following the disaster an emphasis on the often overwhelming demands related to rescues, managing physical injuries and rebuilding infrastructure and communities and an underestimation of the long-term demand for psychosocial services.
Figure 1: Tiered Psychosocial Response to Disasters: supporting the community and individuals post-disaster Modified from IASC Guidelines on Mental Health and Psychosocial Support in Emergency Settings (2007) (p12) and NATO. (2008). Psychosocial Care for People Affected by Disasters and Major Incidents. (p54).
Figure 2: Framework for development and implementation of post-disaster recovery plan. [Modified from World Bank Recovery Planning Processes from Guide to developing disaster recovery frameworks. (2015)].
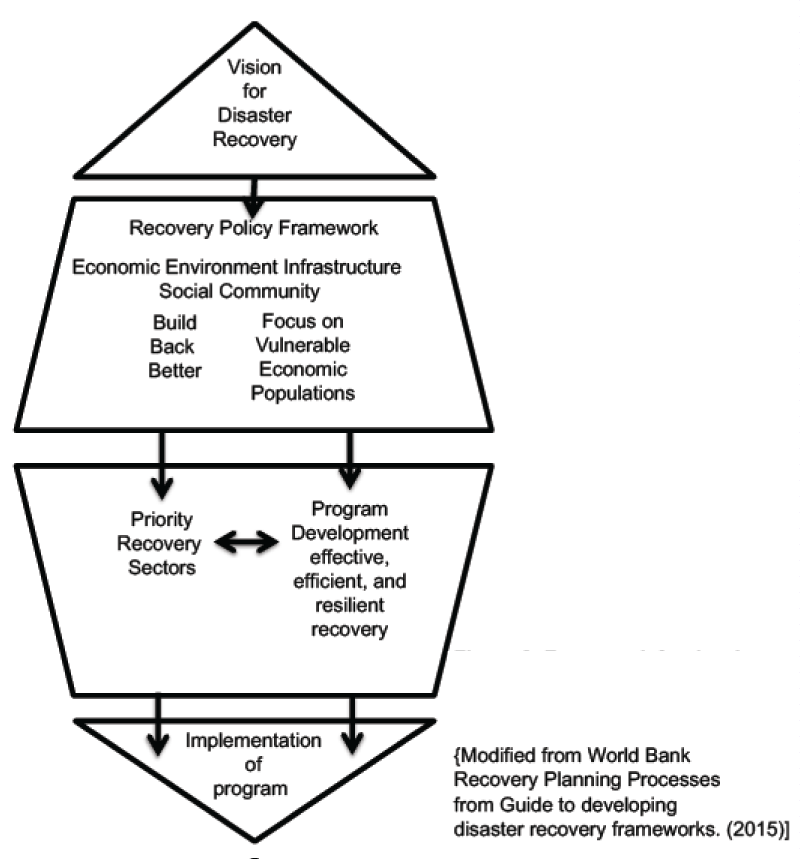
The challenge for governments and other agencies is to reduce the mental health, social and infrastructure burden of natural disasters through public health preparedness through strategies that encompass individuals, organizations, communities, government and political processes. This comprehensive approach requires consideration of urban redesign, use of technological advances (eg meteorology), implementation of cost-effective psychosocial responses that more effectively identify those at-risk, and improved access to evidence-informed care and services appropriate to the needs of affected communities and individuals (Figure 3). The developments in meteorology provide increased predictability of weather and hydrological forecasting [93,94] offering the opportunity to address vulnerability to floods that may occur following the transformation of floodplains through urbanization. Importantly, in conjunction with these developments is the need for more effective communication of risk to organizations and individuals to facilitate a reduction in adverse outcomes particularly in at-risk populations [95-97].
Figure 3: Post-disaster health outcomes – a complex interaction of the event and community. Geo-political and individual factors. Modified from Ursano et al. Ed (2007) p 74.
Identification of populations at risk of adverse mental health outcomes post-disaster through the inclusion of demographic, community socio-economic and health data and weather mapping, hydrological data and hazard mapping [98-100] enables spatial analysis to identify service demands and resource gaps that can increase the likelihood of adverse outcomes [101-107]. This predictive capability is particularly relevant to regions subject to flooding where studies link flood height with the risk of adverse psychological outcomes [69,108]. A Serbian spatial and temporal comparative analysis of vulnerability to natural disasters found that changes in demographic and economic parameters were causally related to the vulnerability risk following a natural disaster [109]. In addition to the demographic and economic factors the inclusion of variables such as alcohol use, availability of health services and the number of individuals on disability pensions enabled the development of geospatial mapping that identified areas with an increased risk of suicide [110].
In contrast to the increasing sophistication of disaster response systems, the mental health and social response demonstrates variability with respect to access to mental health care and evidence-informed treatment programs with services, often not reflective of the needs of individuals [72,111], although Australian disaster response initiatives have gradually adopted a number of innovative approaches that seek to engage at-risk populations and systematically involve communities and sectors such as health and education. E-treatment [112] and school, family interventions and Disaster Recovery Triple P [87,113,114] provide accessible community treatment with the linkage of health and education connecting vulnerable populations. Despite the introduction of these programs following large-scale natural disasters, the demand for services often exceeds the response capability. The discrepancy between the needs of affected communities and availability of resources is a problem relevant to under-developed, developing countries and economies such as Australia, United States and Europe [115,116]. The preparedness of communities and countries to address the social, cultural, economic, and psychological impact of disasters and engage with the transformation of short-term responses to meaningful long-term interventions and sustainable outcomes is influenced by factors such as financial loss, community dislocation and severity of the damage [108,117].
Variability in the capacity to respond, and recognition of the economic, social and mental health consequences of disasters and the scale of events has led countries such as Australia and the European Network for Traumatic Stress to recommend a tiered mental health response across the community. The tiered response ranges from the provision of psychological first aid to evidence-informed interventions provided after a comprehensive assessment [70,118,119]. Inconsistencies in relation to disaster planning, the provision of mental health services and psychosocial care after disaster remain. Methods of screening and diagnosis and the type of interventions [3,120] along with the planning of mental health service delivery following a disaster typically have a general focus rather than on individuals and communities at highest risk for adverse outcomes.
Conclusion
In an era of increasing numbers of natural disasters that confront the capacity of governments, non-government agencies, communities and individuals to respond to the immediate and long-term impacts of disaster there is a necessity as demonstrated by the European Network for Traumatic Stress to adopt a coherent, tiered response that encompasses, assessment, evidence-informed care, and cultural and community responses while addressing the requirements of vulnerable populations such as children, adolescents and those with pre-existing illness [118-121]. Mental health interventions must occur within a partnership framework linked to community and infrastructure redevelopment that has in recent years been approached with increased sophistication as governments focus on addressing economic recovery [122].
The challenge for disaster affected populations that are at significant risk of developing mental illness and social disruption in the immediate and long-term, is the focus on resources and infrastructure redevelopment to the exclusion of social and mental health interventions that assists individual and community recovery. The disaster planning initiated in Queensland after the Floods and Cyclones of 2010-11 adopted a systematic approach that linked public mental health, education sector, non-government organizations, local, state and national authorities, community groups and general practitioners and other primary care providers (psychologists, social workers and occupational therapists). This broad response also engaged with emergency services and infrastructure redevelopment. The post-event planning predicted the adverse psychological impact following the floods and cyclones would exceed available clinical resources. While Queensland has developed a robust structure to address the impact of disasters there remain knowledge and system gaps that impact on the development and implementation of disaster response plans and decisions with respect to resource allocation to meet the psychological needs of affected communities.
The implementation of the post-natural disaster response plan to address the mental health and social impact of the affected Queensland population that was dispersed across a large geographic area provided an opportunity to evaluate the effectiveness of an integrated intervention program that included community-based social interventions, population screening, skills for psychological recovery training program for community clinicians and standardized evaluation and treatment programs delivered by specialized adult and child and adolescent mental health teams.
The disaster response plan aimed to facilitate community resilience building, access to services and address the unmet mental health needs of individuals affected by disasters [43]. The achievement of these goals remains an aspiration for many countries. The focus on immediate response and reconstruction, while important may distract from the importance of the psychosocial response and the necessity to develop models of care that integrate public and mental health planning, response preparedness, and systems such as predictive technology. Disaster health preparedness should integrate services that support the immediate and long-term recovery, a process that may take a number of years (Figure 3). The response to the floods and cyclones in Queensland enabled the development of a systematic evaluation of the program elements that informs future disaster preparedness.
Ethics approval
HREC/14/QPAH/472 – A retrospective evaluation of the outcomes Statewide disaster mental health programs established and delivered following the Cyclones and Floods of 2010-2011.
Results
Vascular risk factors are outlined in table 1: 81% of patients had arterial hypertension, 67% had hypercholesterolemia and about 40% had hypertriglyceridemia, 15 patients out of 90 (17%) had already experienced cerebrovascular events. The table 2 shows the anatomical distribution of the WML. The most frequent sites are the frontal and around the limbic system areas (internal capsule), where lesions were present in 38 and 31 cases respectively. The prefrontal cortex (PFC), which is one of the last territories of the neocortex to develop, in evolution as well as ontogeny, its function is dedicated to the memory, planning, or execution of actions. The PFC can be subdivided in three major region: orbital and medial regions are involved in emotional behavior and lateral region, which is maximally developed he human, provides the cognitive support to the temporal organization of behavior, speech and reasoning. The orbital and medial PFC is the association cortex of the frontal lobe (in primates, it comprises areas 8-13,24,32,46,47) which is well connected with the braimstein and limbic formation, plays a major role in emotional behavior and the control of basic drives. A cardinal function of the lateral PFC is the temporal integration of information for the attainment of prospective behavioral goals. This function of temporal organization is served by several subordinate functions that are closely interwined (e.g., temporal integration, working memory). Much of the connectivity with subcortical structures is reciprocal. Especially well organized topologically are the connections between the PFC and the thalamus. The prefrontal connections with thalamus mediodorsal thalamic nucleus have been used as a criterion for identifying the PFC in a wide variety of species. This is the reason why the discussion of the operation of the PFC is here preceded by the placement of the PFC in a cortical connectionist map of cognitive representations. The study reveals widespread vestibular activations in the motor, visual, and somatosensory cortex; associative parietal cortex; prefrontal cortex; and thalamus and limbic structures. A regulatory control of frontal region over posterior systems for sensation and autonomic functions in a dense, interconnected network was suggested and associative relation within the right hemisphere were proposed to explain links among dizziness, nausea and negative emotions.
References
- Australian Emergency Management Institute. Disaster Health Handbook 1. Attorney-General, editor. Canberra: Commonwealth of Australia; 2011.
- Council of Australian Government. National Strategy for Disaster Resilience: Building our nation's resilience to disasters. Government CoA, editor. Canberra: Attorney-General; 2011.
- NSW Health and University of Western Sydney. NSW Health Disaster Mental Health Manual Sydney: New South Wales Government; 2012.
- Winkworth G. Disaster Recovery: A review of the literature. Dickson, ACT: Institute of Child Protection Studies. 2007. Ref.: https://goo.gl/mf87Cs
- Jin Y, Xu J, Liu D. The relationship between post traumatic stress disorder and post traumatic growth: Gender differences in PTG and PTSD subgroups. Social Psychiatry and Psychiatric Epidemiology. 2014; 49: 1903-1910. Ref.: https://goo.gl/xse4bb
- Becker AE, Kleinman AK. Mental health and the global agenda. The New England Journal of Medicine. 2013; 369: 66-73. Ref.: https://goo.gl/HViRyZ
- Cheng MH. Natural disasters highlight gaps in preparedness. The Lancet. 2009; 374: 1317-1318. Ref.: https://goo.gl/ioJDNX
- Bryant RA, Waters E, Gibbs L, Gallagher HC, Pattison P, et al. Psychological outcomes following the Victorian Black Saturday bushfires. Australian & New Zealand Journal of Psychiatry. 2014; 48: 634-643. Ref.: https://goo.gl/mwwXnR
- Cao H, McFarlane AC, Klimidis S. Prevalence of psychiatric disorder following the 1988 Yun Nan (China) earthquake-the first 5-month period. Social Psychiatry and Psychiatric Epidemiology. 2003; 38: 204-212. Ref.: https://goo.gl/8UL1j8
- Ohta Y, Araki K, Kawasaki N, Nakane Y, Honda S, et al. Psychological distress among evacuees of a volcanic eruption in Japan: A follow-up study. Psychiatry Clinical Neurosciences. 2003; 57: 105-111. Ref.: https://goo.gl/a8igsA
- McNally RJ. Progress and controversy in the study of posttraumatic stress disorder. Annual Review of Psychology. 2003; 54: 229-252. Ref.: https://goo.gl/q1dibT
- Boehnlein JK, Kinzie JD. Commentary. DSM Diagnosis of Posttraumatic Stress Disorder and Cultural Sensitivity: A Response. J Nervous Mental Disease. 1992; 180: 597-599. Ref.: https://goo.gl/K8Z5Nu
- Gersons BP, Carlier IV. Post-traumatic stress disorder: The history of a recent concept. Bri J Psychiatry. 1992; 161: 742-748. Ref.: https://goo.gl/zVrooD
- Parry-Jones B, Parry-Jones WL. Post-traumatic stress disorder: Supportive evidence from an eighteenth century natural disaster. Psychological Medicine. 1994; 24: 15-27. Ref.: https://goo.gl/vpGZP3
- Başoğlu M, Kılıç C, Şalcıoğlu E, Livanou M. et al. Prevalence of Posttraumatic Stress Disorder and Comorbid Depression in Earthquake Survivors in Turkey: An Epidemiological Study. J Traumatic Stress. 2004; 17: 133-141. Ref.: https://goo.gl/1bFJoP
- Chang MC, Chen PF, Lung FW. Anxiety in predicting suicide-related symptom of typhoon disaster victims: a one-year follow-up study in southern Taiwan. The Psychiatric quarterly. 2012; 83: 481-487. Ref.: https://goo.gl/ZrJFtZ
- Zhang Z, Wang W, Shi Z, Wang L, Zhang J. Mental health problems among the survivors in the hard-hit areas of the Yushu earthquake. PLoS ONE. 2012. Ref.: https://goo.gl/WdVwVo
- Norris FH, Murphy AD, Baker CK, Perilla JL. Postdisaster PTSD over four waves of a panel study of Mexico's 1999 flood. J Traumatic Stress. 2004; 17: 283-292. Ref.: https://goo.gl/1n2tmm
- Johannesson KB, Lundin T, Hultman CM, Lindam A, Dyster-Aas J, et al. The effect of traumatic bereavement on tsunami-exposed survivors. J Traumatic Stress. 2009; 22: 497-504. Ref.: https://goo.gl/AzpYnR
- Ali M, Farooq N, Bhatti MA, Kuroiwa C. Assessment of prevalence and determinants of posttraumatic stress disorder in survivors of earthquake in Pakistan using Davidson Trauma Scale. Journal of affective disorders. 2012; 136: 238-243. Ref.: https://goo.gl/MErxM7
- Zhang Y, Ho SMY. Risk factors of posttraumatic stress disorder among survivors after the 512 Wenchuan earthquake in China. PloS one. 2011; 6. Ref.: https://goo.gl/8cd1sa
- Boscarino Ja, Kirchner HL, Hoffman SN, Sartoius J, Adams RE. PTSD and alcohol use after the World Trade Center attacks: a longitudinal study. Journal of traumatic stress. 2011; 24: 515-525. Ref.: https://goo.gl/PSKRJp
- Nordløkken A, Pape H, Wentzel-Larsen T, Heir T. Changes in alcohol consumption after a natural disaster: A study of norwegian survivors after the 2004 southeast asia tsunami. BMC Public Health. 2013; 13: 58. Ref.: https://goo.gl/7F5z7k
- Cerdá M, Tracy M, Galea S. A prospective population based study of changes in alcohol use and binge drinking after a mass traumatic event. Drug and alcohol dependence. 2010; 115: 1-8. Ref.: https://goo.gl/9mzNzU
- North CS, Ringwalt CL, Downs D, Derzon J, Galvin D. Postdisaster course of alcohol use disorders in systematically studied survivors of 10 disasters. Archives of general psychiatry. 2011; 68: 173-180. Ref.: https://goo.gl/DJp9uU
- Chou YJ, Huang N, Lee CH, Tsai SL, Tsay JH, et al. Suicides after the 1999 Taiwan earthquake. International journal of epidemiology. 2003; 32: 1007-1014. Ref.: https://goo.gl/gn2ffs
- Maeda M, Oe M, Bromet E, Yasumura S, Ohto H. Fukushima, mental health and suicide. Journal of Epidemiology and Community Health, 2016; 70: Ref.: https://goo.gl/7XkbdZ
- Kõlves K, Kõlves KE, De LD. Natural disasters and suicidal behaviours: a systematic literature review. Journal of affective disorders. 2013; 146: 1-14. Ref.: https://goo.gl/mtkMAQ
- Krug EG, Kresnow MJ, Peddicord JP, Dahlberg LL, Powell KE, et al. Retraction: Suicide after natural disasters. The New England Journal of Medicine. 1999; 340: 148-149. Ref.: https://goo.gl/eokYC7
- Gordon KH, Bresin K, Dombeck J, Routledge C, Wonderlich Ja. The Impact of the 2009 Red River Flood on Interpersonal Risk Factors for Suicide. Crisis. 2011; 32: 52-55. Ref.: https://goo.gl/t8zsgL
- Harville EW, Taylor CA, Tesfai HT, Xiong X, Buekens P. Experience of Hurricane Katrina and reported intimate partner violence. J Interpersonal Violence. 2011; 26: 833-845. Ref.: https://goo.gl/GWoQ14
- Zahran S, Peek L, Snodgrass JG, Weiler S, Hempel L. Economics of Disaster Risk, Social Vulnerability, and Mental Health Resilience. Risk Analysis. 2011; 31: 1107-1119. Ref.: https://goo.gl/LsF49p
- Zotti ME, Williams AM, Robertson M, Horney J, Hsia J. Post-disaster reproductive health outcomes. Matern Child Health J. 2013; 17: 783-796. Ref.: https://goo.gl/ARdFZW
- Venn D. Helping displaced workers back into jobs after a natural disaster: Recent Experiences In Oecd Countries. 2012. Ref.: https://goo.gl/CenKX6
- Julca A. Natural disasters with un-natural effects: Why? J Economic Issues. 2012; 46: 499-510. Ref.: https://goo.gl/UByXnu
- Armaş I. Multi-criteria vulnerability analysis to earthquake hazard of bucharest, Romania. Natural Hazards. 2012; 63: 1129-1156. Ref.: https://goo.gl/gop5Pn
- Cerdá M, Vlahov D, Tracy M, Galea S. Alcohol use trajectories among adults in an urban area after a disaster: evidence from a population-based cohort study. Addiction. 2008; 103: 1296-1307. Ref.: https://goo.gl/nKtgRH
- Mason V, Andrews H, Upton D. The psychological impact of exposure to floods. Psychology, Health & Medicine. 2010; 15: 61-73. Ref.: https://goo.gl/ZYW3gL
- Ohl CA, Tapsell S. Flooding and human health. British Medical Journal. 2000; 321. Ref.: https://goo.gl/Swt82w
- Hobfoll SE, Watson P, Layne CM, Maguen S, Neria Y, et al. Five essential elements of immediate and mid-term mass trauma intervention: Empirical evidence. Psychiatry. 2007; 70: 283-315. Ref.: https://goo.gl/NYbhtU
- NATO. Psychosocial Care for People Affected by Disasters and Major Incidents; A Model for Designing, Delivering and Managing Psychosocial Services for People Involved in Major Incidents, Conflict, Disasters and Terrorism. North Atlantic Treaty Organization. 2008. Ref.: https://goo.gl/nsxj6f
- North CS, Pfefferbaum B. Mental health response to community disasters: A Systematic Review. 2013; 310: 507-518. Ref.: https://goo.gl/ZFdS1b
- Schoenbaum M, Butler B, Kataoka S, Norquist G, Springgate B, et al. Promoting mental health recovery after hurricanes katrina and rita: What could we done at what cost? Archives of general psychiatry. 2009; 66: 906-914. Ref.: https://goo.gl/mw9Qrc
- Ursano RJ, Fullerton CS, Weisaeth L, Raphael B. Textbook of disaster psychiatry. Cambridge University Press. 2017. Ref.: https://goo.gl/zRyNGQ
- Blumenfield M, Ursano RJ. Intervention and resilience after mass trauma. Cambridge University Press. 2008. Ref.: https://goo.gl/Srx367
- Gow K, Celinski MJ. Mass trauma: Impact and recovery issues. Nova Science Publishers. 2013. Ref.: https://goo.gl/Jh9cRP
- Whittle R, Walker M, Medd W, Mort M. Flood of emotions: Emotional work and long-term disaster recovery. Emotion, Space and Society. 2012; 51: 60-69. Ref.: https://goo.gl/3RDdWd
- Ehlers A, Hackmann A, Manley J, Brady F, Clark DM, et al. Implementation of cognitive therapy for PTSD in routine clinical care: Effectiveness and moderators of outcome in a consecutive sample. Behav Res Ther. 2013; 51: 742-752. Ref.: https://goo.gl/Afx5hz
- Gallagher MW, Payne LA, White KS, Shear KM, Woods SW, et al. Mechanisms of change in cognitive behavioral therapy for panic disorder: The unique effects of self-efficacy and anxiety sensitivity. Behav Res Ther. 2013; 51: 767-777. Ref.: https://goo.gl/riVDos
- Grist R, Cavanagh K. Computerised cognitive behavioural therapy for common mental health disorders, what works, for whom under what circumstances? A systematic review and meta-analysis. J Contemporary Psychotherapy. 2013; 43: 243-251. Ref.: https://goo.gl/G2ZXdM
- Ma SH, Teasdale JD. Mindfulness-based cognitive therapy for depression: Replication and exploration of differential relapse prevention effects. J Consult Clin Psychol. 2004; 72: 31-40. Ref.: https://goo.gl/Yh7JYH
- Jacobs GA. The development of a national plan for disaster mental health. Professional Psychology: Research and Practice. 1995; 26: 543-549. Ref.: https://goo.gl/qNmGDq
- Dieltjens T, Moonens I, Praet KV, Buck ED, Vandekerchove P. A systematic literature search on psychological first aid: Lack of evidence to develop guidelines. PLoS One. 2014; 9. Ref: https://goo.gl/aR1rnm
- Forbes D, Lewis V, Varker T, Phelps A, O’Donnell M, et al. Psychological first aid following trauma: Implementation and evaluation framework for high-risk organizations. Psychiatry. 2011; 74: 224-239. Ref.: https://goo.gl/JRVctn
- Ruzek JI, Brymer MJ, Jacobs AK, Layne CM, Vernberg EM, et al. Psychological first aid. J Mental Health Counseling. 2007; 29: 17-49. Ref.: https://goo.gl/fLHDk1
- Vernberg EM, Steinberg AM, Jacobs AK, Brymer MJ, Watson PJ, et al. Innovations in disaster mental health: Psychological first aid. Professional Psychology: Research and Practice. 2008; 39: 381-388. Ref.: https://goo.gl/5x9iHT
- Goenjian AK, Karayan I, Pynoos RS, Minassian D, Najarian LM, et al. Outcome of psychotherapy among early adolescents after trauma. Am J Psychiatry. 1997; 154: 536-542. Ref.: https://goo.gl/ArphxP
- Shooshtary MH, Panaghi L, Moghadam JA. Outcome of cognitive behavioral therapy in adolescents after natural disaster. J Adolesc Health. 2008; 42: 466-472. Ref.: https://goo.gl/FPKwpQ
- Başoğlu M, Livanou M, Şalcıoğlu E, Kalender D. A brief behavioural treatment of chronic post-traumatic stress disorder in earthquake survivors: results from an open clinical trial. Psychol Med. 2003; 33: 647-654. Ref.: https://goo.gl/Y6hLUw
- Bassilios B, Reifels L, Pirkis J. Enhanced primary mental health services in response to disaster. Psychiatric Services. 2012; 63: 868-874. Ref.: https://goo.gl/kBRLz7
- Norris FH, Friedman MJ, Watson PJ. 60,000 disaster victims speak: Part II. Summary and implications of the disaster mental health research. Psychiatry. 2002; 65: 240-260. Ref.: https://goo.gl/Ws1ctE
- Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E, et al. 60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981-2001. Psychiatry. 2002; 65: 207-239. Ref.: https://goo.gl/bAzXL3
- Druss BG, Satcher D. Bridging Mental Health and Public Health. Prev Chronic Dis. 2010; 7. Ref.: https://goo.gl/V7N3QB
- Satcher D, Friel S, Bell R. Natural and Manmade Disasters and Mental Health. JAMA. 2007; 298: 2540-2542. Ref.: https://goo.gl/xiYWwN
- Johannesson KB, Michel PO, Hultman CM, Lindam A, Arnberg F, et al. Impact of exposure to trauma on posttraumatic stress disorder symptomatology in Swedish tourist tsunami survivors. J Nerv Ment Dis. 2009; 197: 316-323. Ref.: https://goo.gl/SjGrvt
- NHS. Planning for the psychosocial and mental health care of people affected by major incidents and disasters: Interim National Strategic Guidance. Ref.: https://goo.gl/n9gW7d
- WHO. The determinants of health Geneva. Ref.: https://goo.gl/wkcSpM
- Department of Health and Human Services. Mental Health All-Hazards Disaster Planning Guidance. Rockville: Center for Mental Health Services, Substance Abuse and Mental Health Services Administration. 2003. Ref.: https://goo.gl/TjdAUx
- Malilay J, Heumann M, Perrotta D, Wolkin AF, Schnall AH, et al. The role of applied epidemiology methods in the disaster management cycle. Am J Public Health. 2014; 104: 2092-2102. Ref.: https://goo.gl/M6r6Wv
- Reifels L, Naccarella L, Blashki G, Pirkis J. Examining disaster mental health workforce capacity. Psychiatry. 2014; 77: 199-205. Ref.: https://goo.gl/bD9S8T
- Logue JN. The public health response to disasters in the 21st century: reflections on Hurricane Katrina. J Environ Health. 2006; 69: 9-13. Ref.: https://goo.gl/EMAAeB
- Norris FH, Bellamy ND. Evaluation of a national effort to reach Hurricane Katrina survivors and evacuees: the crisis counseling assistance and training program. Adm Policy Ment Health. 2009; 36: 165-175. Ref.: https://goo.gl/szHKxe
- Zahran S, Brody SD, Peacock WG, Vedlitz A, Grover H. Social vulnerability and the natural and built environment: A model of flood casualties in texas. Disasters. 2008; 32: 537-560. Ref.: https://goo.gl/mjN5E2
- Victorian Bushfires Royal Commission. Victoria State Government. 2009. https://goo.gl/ff5QNg
- Caruana C. Picking up the pieces: Family functioning in the aftermath of natural disaster. Australian Government. 2010. Ref.: https://goo.gl/ZamQMf
- Berry HL, Hogan A, Owen J, Rickwood D, Fragar L. Climate change and farmers’ mental health: Risks and responses. Asia-Pacific J Public Health. 2011; 23: 119S-1132S. Ref.: https://goo.gl/9ZhAiS
- Disaster Health. Australian emergency management handbook and manual series. General A, editor. Canberra: Australian Government. 2011. 109.
- Queensland Government. Disaster Management Brisbane: Queensland Government; 2015. Queensland Government. 2013-2014 Queensland State Disaster Management Plan Brisbane. 2013.
- World Health Organisation. World Health Organisation Guidance for Health Sector Assessment to Support the Post Disaster Recovery Process. 2010. Ref.: https://goo.gl/7bwDAU
- Arklay T. Queensland's state disaster management group: An all agency response to an unprecedented natural disaster. Australian J Emergency Management. 2012; 27. Ref.: https://goo.gl/41qe2S
- RedCross. Queensland floods 2011 Australia: Australian Red Cross; 2018.
- Australian Army. Operation Queensland Flood Assist 2011: Department of Defence; 2011.
- Queensland Reconstruction Authority. Queensland Reconstruction Authority Strategic Plan. 2012. Ref.: https://goo.gl/VdiWq6
- Queensland Reconstruction Authority. Queensland Reconstruction Authority Progress Report Brisbane Queensland Reconstruction Authority. 2013. Ref.: https://goo.gl/s2x2h4
- Wade D, Crompton D, Howard A, Stevens N, Metcalf O, et al. Evaluation of a post-disaster mental health training program. Disaster Health. 2015; 2: 138-145. Ref.: https://goo.gl/ZwHhNq
- Mc Dermott BM, Cobham VE. A stepped-care model of post-disaster child and adolescent mental health service provision. Eur J Psychotraumatology. 2014; 5. Ref.: https://goo.gl/ur1VES
- Raphael B, Dunsmore JC, Wooding S. Terror and trauma in bali: Australia's mental health disaster response. Haworth Maltreatment & Trauma Press. 2005; 9: 245-256. Ref.: https://goo.gl/B118id
- Reifels L, Pietrantoni L, Prati G, Kim Y, Kilpatrick DG, et al. Lessons learned about psychosocial responses to disaster and mass trauma: An international perspective. Eur J Psychotraumatology. 2013; 4. Ref.: https://goo.gl/ztbcKi
- Munich RE. Significant natural disasters since 1980: Munich Reinsurance America. 2014. Ref.: https://goo.gl/nEsYJ4
- Inter-Agency Standing Committee (IASC). IASC Guidelines on Mental Health and Psychosocial Support in Emergency Settings. 2007.
- GFDRR (Global Facility for Disaster Reduction and Recovery), Guide to developing disaster recovery frameworks. Sendai Conference; Washington DC: Global Facility for Disaster Reduction and Recovery. 2015. Ref.: https://goo.gl/61yVV5
- Roy C, Kovordányi R. Tropical cyclone track forecasting techniques - A review. Atmospheric Research. 2012; 104-105: 40-69. Ref.: https://goo.gl/7AidD6
- Zarnani A, Musilek P, Heckenbergerova J. Clustering numerical weather forecasts to obtain statistical prediction intervals. Meteorological Applications. 2014; 21: 605-618. Ref.: https://goo.gl/e7ekTF
- Neal J, Keef C, Bates P, Beven K, Leedal D. Probabilistic flood risk mapping including spatial dependence. Hydrological Processes. 2013; 27: 1349-1363. Ref.: https://goo.gl/KwCc8B
- Schröter K, Kreibich H, Vogel K, Riggelsen C, Scherbaum F, et al. How useful are complex flood damage models? Water Resources Research. 2014; 50: 3378-3395. Ref.: https://goo.gl/hYJSM5
- Stephens E, Cloke H. Improving flood forecasts for better flood preparedness in the UK (and beyond). Geographical J. 2014; 180: 310-316. Ref.: https://goo.gl/8ZpCZA
- Department of Natural Resources and Mines. Department of Natural Resources and Mines - Interactive Floodcheck map Brisbane: Queensland Government; 2015.
- Poompavai V, Murugaiya R. Geospatial analysis for coastal risk assessment to cyclones. J Indian Society Remote Sensing. 2013; 41. Ref.: https://goo.gl/JHgQ6U
- Honert RCVD, McAneney J. The 2011 brisbane floods: Causes, impacts and implications. Water. 2011; 3: 1149-1173. Ref.: https://goo.gl/nGSRKN
- Curtis A, Mills JW, Kennedy B, Fotheringham S, McCarthy T. Understanding the geography of Post‐Traumatic stress: An academic justification for using a spatial video acquisition system in the response to hurricane katrina. J Contingencies and Crisis Management. 2007; 15: 208-219. Ref.: https://goo.gl/RC5ZGJ
- Earnest A, Tan SB, Shahidah N, Ong ME. Geographical variation in ambulance calls is associated with socioeconomic status. Academic Emergency Medicine. 2012; 19: 180-188. Ref.: https://goo.gl/RNq2e4
- Salinas-Pérez JA, García-Alonso CR, Molina-Parrilla C, Jorda-Sampietro E, Salvador-Carulla L, et al. Identification and location of hot and cold spots of treated prevalence of depression in catalonia (Spain). Int J Health Geographics. 2012; 11. Ref.: https://goo.gl/VyLgc3
- Jagodic HK, Rokavec T, Agius M, Pregelj P. Availability of mental health service providers and suicide rates in slovenia: A nationwide ecological study. Croat Med J. 2013; 54: 444-452. Ref.: https://goo.gl/PYmcKA
- Aubrecht C, Özceylan D, Steinnocher K, Freire S. Multi-level geospatial modeling of human exposure patterns and vulnerability indicators. Natural Hazards. 2013; 68: 147-163. Ref.: https://goo.gl/d3atWU
- Gros DF, Price M, Gros KS, Paul LA, McCauley JL, et al. Relations between loss of services and psychiatric symptoms in urban and non-urban settings following a natural disaster. J Psychopathol Behav Assess. 2012; 34: 343-350. Ref.: https://goo.gl/PpfnEF
- Waring S, Zakos-Feliberti A, Wood R, Stone M, Padgett P, et al. The utility of geographic information systems (GIS) in rapid epidemiological assessments following weather-related disasters: Methodological issues based on the tropical storm allison experience. Int J Hygiene Environmental Health. 2005; 208: 109-116. Ref.: https://goo.gl/sWCpvZ
- Paranjothy S, Gallacher J, Amlôt R, Rubin GJ, Baxter T, et al. Psychosocial impact of the summer 2007 floods in England. BMC Public Health. 2011; 11: 145. Ref.: https://goo.gl/FtBpv5
- Kovačević-Majkić J, Panić M, Miljanović D, Miletic R. Vulnerability to natural disasters in serbia: Spatial and temporal comparison. Natural Hazards. 2014; 72: 945-968. Ref.: https://goo.gl/pfMfWc
- Balint L, Dome P, Daroczi G, Gonda X, Rihmer Z. Investigation of the marked and long-standing spatial inhomogeneity of the hungarian suicide rate: A spatial regression approach. J Affect Disord. 2014; 155: 180-185. Ref.: https://goo.gl/NFG4yq
- Norris FH, Rosen CS. Innovations in disaster mental health services and evaluation: National, state, and local responses to hurricane katrina (introduction to the special issue). Administration and Policy in Mental Health and Mental Health Services Research. 2009; 36: 159-164. Ref.: https://goo.gl/DW6KAP
- Kavanagh D. On Track Flood and Storm Recovery. Ref.: https://goo.gl/7riqWD
- Cobham V, Mc Dermott B, Sanders M. The development and evaluation of Disaster Recovery Triple P: After the disaster. 2011.
- University of Queensland. Natural disasters take an emotional toll on kids Washington DC. 2013.
- Choudhury WA. Quraishi FA, Haque Z. Mental health and psychosocial aspects of disaster preparedness in bangladesh. Int Rev Psychiatry. 2006; 18: 529-535. Ref.: https://goo.gl/s1N8Ge
- Raphael B, Ng CH. Disaster mental health preparedness and response: Asia‐Pacific perspectives. Asia‐Pacific Psychiatry. 2011; 3: 163-166. Ref.: https://goo.gl/BTzKmw
- Dominici F, Levy JI, Louis TA. Methodological challenges and contributions in disaster epidemiology. Epidemiol Rev. 2005; 27: 9-12. Ref.: https://goo.gl/M54rSw
- Bisson JI, Tavakoly B, Witteveen AB, Ajdukovic D, Jehel L, et al. TENTS guidelines: Development of post-disaster psychosocial care guidelines through a delphi process. Br J Psychiatry. 2010; 196: 69-74. Ref.: https://goo.gl/181hmh
- Australian Centre for Posttraumatic Mental Health. Recovery (SPR) Training and Support Program: Final Report for Queensland Health. Melbourne: ACPMH; 2013.
- Witteveen AB, Bisson JI, Ajdukovic D, Arnberg FK, Johannesson KB, et al. Post-disaster psychosocial services across Europe: The TENTS project. Social Science & Medicine. 2012; 75: 1708-1714. Ref.: https://goo.gl/D2TJgU
- Stein DJ, Friedman MJ, Blanco C. Disaster public mental health. Chichester, UK: John Wiley & Sons, Ltd. 2011.Ref.: https://goo.gl/pN84cy
- Queensland: Recovery and Reconstruction in the Aftermath of the 2010/2011 Flood Events and Cyclone Yasi. Brisbane: Queensland Government; 2011. Ref.: https://goo.gl/a3xtnc