Case Report
May we feed cancer?

Maria Grazia Spurio*
Psychotherapist, Master in Neuropsychiatry, Neuropsychology and Forensic Psychology, Director of Educational and Psychological Center “Genius Academy”, Via Carlo Arturo Jemolo, 83 00156, Rome, Italy*Address for Correspondence: Maria Grazia Spurio, Psychotherapist, Master in Neuropsychiatry, Neuropsychology and Forensic Psychology, Director of Educational and Psychological Center “Genius Academy”, Via Carlo Arturo Jemolo, 83 00156, Rome, Italy, Email: [email protected]
Dates: Submitted: 28 December 2017; Approved: 09 February 2018; Published: 12 February 2018
How to cite this article: Spurio MG. May we feed cancer? Insights Depress Anxiety. 2018; 2: 001-006. DOI: 10.29328/journal.ida.1001005
Copyright License: © 2018 Spurio MG. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Food; Cancer; Depression
Abstract
The patient with an oncological disease presents a series of discomforts related to the psychological sphere such as depression, pain, sense of usefulness, anger, but also inconveniences related to food sphere. Neoplastic disease interferes with eating behaviour for several reasons. The communication of the diagnosis can create a state of anorexia as a result of the shock; certain tumours of the gastrointestinal tract-gold (mouth, esophagus, stomach, colon and rectum, but also pancreas and liver) are directly responsible for the possible alteration of food intake; alteration in eating behaviour may be secondary to the main therapeutic treatments. The link between food and cancer is not only evident in case of disease, but also in case of prevention, in fact a growing number of studies indicates more an more clearly the close correlation between a healthy diet and prevention of oncological diseases although at present time it is not still possible to give definitive results. The diagnosis of a person is like a melody in which some notes are repeated but their combination is almost infinite, because each person has different eating needs, as well as different psychological needs, and the starting point for a good professional must necessarily be a ‘customized’ diagnosis. This ‘diagnosis of well-being’, tailor-made for each person, involves professionals in both the food and psychological and behavioural sectors, since the individual needs have to be evaluated globally.
Finally, the professionals of human behaviour in food consumption, and the chemical and science processing experts, have the duty not to limit themselves to a single refusal against the use of certain foods, but framing the phenomenon in a wider perspective and, as experts of human health, to propose alternatives.
Introduction
The challenge for the professionals
The real challenge for a doctor, dietitian, or psychotherapist is to welcome and take charge of that part of reality, discomfort or illness brought into the attention of the professional by the patient, without falling into the easy trap of focusing one’s intervention only on the restricted part linked to disease. The patient is not a simple container of discomfort or disease related to a specific organ to be healed. The stomach, the heart or the lungs, as well as specific brain areas such as the limbic ones and the prefrontal cortex don’t exist if not as closely connected and interacting with the rest of the body and mind.
So the real challenge for a serious professional who works in the field of human health is to have the enthusiasm and ability to welcome people in their full complexity and individuality [1]. It is now necessary to speak of discomfort and disease as a part of a bigger and more complex bio-psycho-social phenomenon, otherwise the discussion on this theme would be purely academic, like an artificial labeling.
To understand how deeply is rooted this type of Cartesian mentality, it can be mentioned the sectored and non holistic way to think which we spontaneously face for social and cultural reasons. When we deal with food, for example, we generally tend to speak of caloric value and of nutritional intake of each food expressed in weights and other measurements, such as content of vitamins, carbohydrates or sugar.
A widespread trend, both in nutrition and medicine in general, maybe for convenience and exigency of simplification, is therefore to divide, to split, so, when one needs refer to the nutritional provision of a food the values are reduced in terms of fats, carbohydrates and calories, forgetting in this way that the whole is not only the simple sum of the parts, of the single nutritive elements, because the experience of eating is made of the setting, the appearance, and the flavour as well.
Each person tells a unique story
The bioenergetic diet makes us aware of how much is important the holistic concept of the whole, as well as sensitizes us to the concept of individuality and specificity. Each individual has unique and unrepeatable characteristics, therefore, also in the field of nutrition it is not only impossible but also dangerous to think about a diet which is the same for everyone. On the contrary one should always start from an accurate diagnosis of the person, that makes possible to identify which is the most suitable food to the person whose care is provided, such as type of cooking and specific times of day when it is preferable to eat or not eat certain foods. Beyond these considerations, since each nutritional principle has a deep impact not only on the health of the individual but also on one’s psychological sphere, because of the chimicals released from every food, a serious professional must take into consideration all the aspects of the psychological sphere of the individual.
Only in this way it is possible to get the optimal diet for the single person and suitable for a precise period of his-her life. The same fundamental principle should be applied when one deals of psychological and mental aspect of a person. There aren’t two individuals for which the same psychotherapy fits well, because there aren’t two identical persons with equal situations, because”each person is a unique universe and the body is the place where mind and body meet in a unique and unrepeatable alchemy” [1,2].
So for therapists, the mere knowledge of things is not enough, one needs enthusiasm, sense of observation, desire to understand and to help, ethics and creativity.
Erickson [3] used successfully the pet therapy in treating a schizophrenic patient, because he integrated with imagination and genius the situation pertaining to the reality of his patient with a little dog in order to overcome some of the typical communication difficulties of schizophrenic patients.
In fact the problem is that in general schizophrenics, do not do things directly but triangulated into something different, for example, through their voices. The therapist must communicate indirectly or triangulate so as to meet patients in their own frame of reference [3]. Erickson set out to achieve indirect communication using pet therapy (assisted by animals) taking a dog for his schizophrenic patient [2].
Each patient therefore presents himself-herself with his/her unique history [4] stitched together by his particular way of understanding life. Attitudes, behaviour and personality are a consequence of DNA, a genetic code that, however, has been combining and recombining each time with personal experiences, in a recursive cycle that is redefined from time to time by new experiences.
The failures, the achievements, sorrows, the loss in general up to the bereavement change the experiences of an individual but also his way of experiencing events and relate to them.
For example the death of a loved one can be heart breaking for those left behind, and indeed, bereavement is associated not only with adverse health effects but also with a higher risk of dying oneself. Not surprisingly, its consequences have been the subject of much psychological enquiry, with a major interest in shedding light on how one adapts, who is most at risk, and why [5].
The cancer patient
It is evident, therefore, how is fundamental for a psychotherapist not to forget the importance of these considerations, moreover when the patient has an oncological disease.
The patient with an oncological disease, in fact, presents a series of discomforts related to the psychological sphere such as depression, pain, sense of usefulness, anger, but also inconveniences related to food sphere. Neoplastic disease interferes with eating behaviour for several reasons. The communication of the diagnosis can create a state of anorexia as a result of the shock; certain tumours of the gastrointestinal tract-gold (mouth, esophagus, stomach, colon and rectum, but also pancreas and liver) are directly responsible for the possible alteration of food intake; alteration in eating behaviour may be secondary to the main therapeutic treatments. In case of surgery the psychological condition, the sense of wellbeing, the desire to eat and the absorption of nutrients can be seriously influenced by the intervention itself.
In patients receiving chemotherapy, many medications cause nausea, vomiting, constipation, diarrhoea, mucosal alteration and difficulty with chewing. Finally, also during radiotherapy there could be temporary and / or permanent disorders. Temporary ones are the same as induced by chemotherapy, while the permanent ones could cause alteration of taste receptors, the secondary dysphagia in fibrotic processes of the pharynx and esophagus, strictures and / or fistulae that can be formed in the gastro-intestinal tract. Moreover, in the therapeutic process of cancer patients, feeding behaviour could also be influenced by psychological problems. Especially anorexia, nausea and anticipatory vomiting closely interact with depressive syndromes, anxious, with psychiatric disorders and in general by emotions such as fear, anger, despair, a sense of disability and mistrust. For all these reasons, a fair, accurate and healthy diet is important for those who are living complex diseases such as cancer.
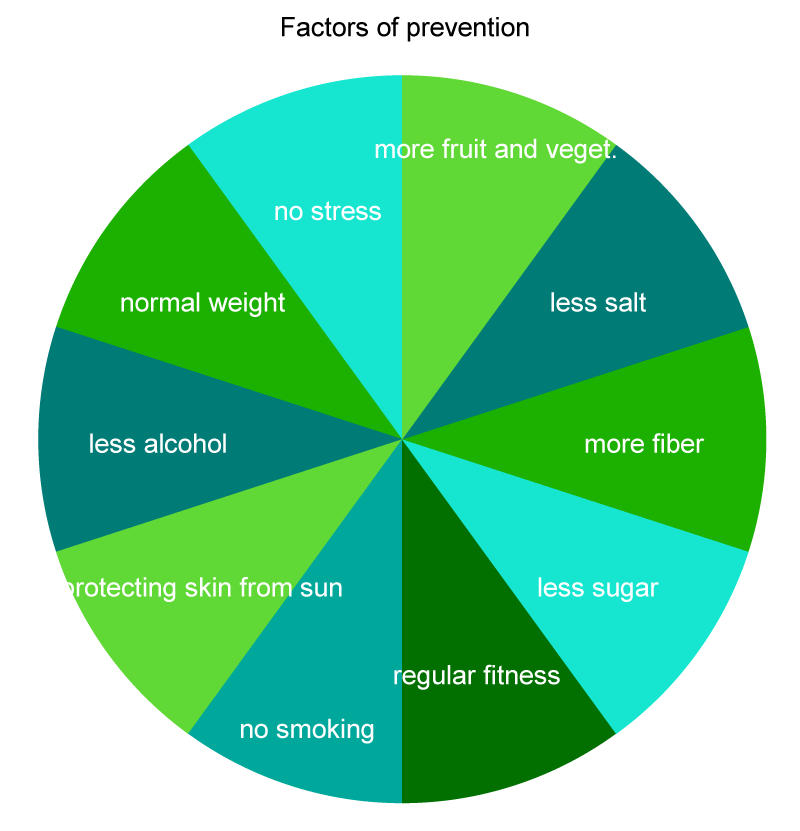
According to many studies, it seems that the typical dietary habits of Americans has a connection with the development of tumors. Too much sugar, too much meat, too many industrially refined foods increase the risk of getting sick, while whole grains, legumes and vegetables have a protective effect. On the contrary, according with the recommendations of world cancer research fund international (www.wcrf.org) with an healthy lifestyle it is possible to prevent about a third of the tumors and the table shows how many important factors have to be taken into consideration in order to set a ‘program of prevention’ (Figure 1).
Another aspect to consider is that in recent decades, depression and mood disorders in general have seen a strong growth. The prevalence of major depressive disorder in adults is 10-25% in the female gender, compared to 5-12% in males [6]. The causes are various (social environment, genetic predisposition, early emotional relationships, etc.).
About the relationship between the onset of an illness and immune resistance we should mention the study conducted at the University of Chicago by Leah Pyter and colleagues (2009). The researchers have shown that the mental condition of depression is not only the consequence of the disease, and not even of a particularly debilitating treatment such as chemotherapy. This would confirm the existence of complex relationships between the immune system and tumors and depression. The negative effects of a depression state on the immune system have been known for a long time, but in recent times, researchers around the world have shown that the path may be the reverse, in fact the activation of the immune system may produce depression, anxiety and cognitive disorders, going through a systemic inflammatory condition that affects the whole ‘body. A real mind and body circularity.
A body that thinks a mind that feels
The latest scientific researches have emphasized that the entire body thinks, because every single cell hears, and feels emotion. There is a sort of body and mind functional identity, which is different in each person, because each person is a unique universe, and the body is the place where mind and body meet in a unique and unrepeatable alchemy. So, if it is true that only in the body the secret of its potential for development and transformation is well hidden, it is also true that this secret is unique for each of us. According to Psiconeuroendocrino immunology (PNEI), that studies the relationship between the fluctuations of hormones and human behaviour, it seems demonstrated that the psyche acts on the body.
When one eats too much sugar the insulin starts to circulate, which however in these cases is evaluated by our body as a sort of “remedial intervention” and “emergency”, for this reason in our organism an altered capacity of the pancreas to produce insulin is determined. This situation of altered functionality, in addition to the fact that it could cause the type II of diabetes, also determines a situation of organic predisposition of inflammatory type.
The pathological consequences of this inflammatory situation can go from colitis to cancer, but as if that were not enough, and as a further demonstration of the indivisible nature of the physiological and psychological causes, this altered organic functionality also determines an increase of body weight, and, consequently, a psychological behaviour strictly connected with the relationship with altered food. The weight gain is also associated with a lowering of insulin levels, which will make, once again, one feel a false sense of hunger. This is false because it doesn’t correspond to a real need, but which, however, will move one to eat again fueling the psychological chemical dysfunctional loop. Therefore we can rightly speak of a link between depression, food and cancer, because frequent insulin surges lead to a continuous mood changes, confused state of mind, frequent fatigue and toxic and negative thoughts that can change into depression.
Moreover, the sense of hunger drives to distorted eating behaviours such as binge eating, which, in turn, generates feelings of guilt and frustration. If in the subsequent meals one continues to eat high-glycaemic foods, he-she would gain weight and consequently the general health conditions would worsen, with additional frustrations, social difficulties, physical tiredness sensations, thoughts of failure. All these symptoms partially coincide with those defined by the DSM IV-TR (diagnostic and statistical Manual of mental disorders) for the diagnosis of major depression. A shortage of sugar slows down the movements, get feeling tired, irritable, vitality decreases, there is a low inclination to social life. In 2005 Markku Timonen [7] published an interesting scientific work on the marked correlation between insulin resistance and depression. The physical activation due to stress is represented by a curve in the shape of an inverted U [8]. A sequence of stressful events with high impact, if repeated during a long period, could bring down, making feel depressed, tired, lacking any perspective. When stress levels are high and protracted this can result in a glucose research and a subsequent search of sweets or other foods rich of sugar. Eating too much cause fat increase, along with all the negative effects of stress: immune inhibition, sleep disturbances, impaired memory, increase in free radicals and reduction of vitamin C, depression. In this scenario, a wrong diet, consisting of concentrates and refined sugars (sweets, soft drinks, ice cream, juices, jams, etc..), will only worsen the situation resulting in an additional risk factor for the development of depressive states and cancer.
A growing number of studies indicates more and more clearly the close correlation between a healthy diet and prevention of oncological diseases although at present time it is not still possible to give the definitive details. The American Institute for Cancer Research [9] has calculated that wrong eating habits are responsible for about three out of ten tumors. A further aspect which is necessary to briefly mention concerns the presence in foods of substances that foster the disease: the nitrites and nitrates used for the preservation of meats, for example, seem to have a connection with the emergence of cancer of the stomach, so that in Italy it seems that the disease is more widespread in regions where the consumption of these products is greater. So, from an holistic point of view, we can affirm that, first of all, the food is not necessarily harmful in itself, but it may be contaminated with substances such as aflatoxins, released by certain molds in corn or other grains and legumes badly preserved. In some countries the developing of aflatoxins is responsible for a significant number of gut cancer. Thus, in this case, instead of demonizing certain foods, the professionals of human behavior in food consumption, and the chemical and science processing experts as well, have the duty not to limit themselves to a single refusal against the use of certain foods, but they could frame the phenomenon in a wider perspective and, as experts of human health, propose alternatives for the health as regard the methods of cultivation, storage, processing, production and everything appropriate for the production of a healthy food.
Conclusion
The long road to win against two of the main causes of many of our sufferings, cancer and depression, has begun long time ago. Already in 1877, Sir James Paget in his study on Surgical Pathology wrote a sentence that it is still possible to agree with: “There are cases in which deep anxiety, hopelessness, disappointment, are so promptly followed by growth and an increase in cancer, that we can hardly doubt that mental depression is an additional burden together with other influences which affect the growth of the cancerous constitution” [10].
Where are we today, along this road? We have no definitive data to assert that stress is a cause of cancer, but we can affirm that stress, dejection, depression and states of deep and prolonged psychological distress, are a path genetic cofactor. It is probable that the whole of neuroendocrine and immune changes that occur in an organism in a state of deep depression may facilitate the discovery of predispositions to somatic diseases. All that lead us to the starting point: the real challenge for a serious professional who works in the field of human health is to have the curiosity, enthusiasm and ability to welcome people in their full complexity and individuality [11]. It is not possible to arbitrarily isolate and select just one aspect of one’s life from all over the rest, forgetting the complex web of social and psychological, feeding and physiological correlations that serve as a contributory cause to the events of one’s life. Therefore, a person is made of the interaction of all these elements, and much more. And when a patient presents in psychotherapist study he/she not only brings a single need, but tells a story of a person, that never and never again should be dismembered and split for academic convenience, on the contrary, it must be embraced it in its entirety and peculiarity of unique and fascinating story, a story that therapists have an ethical responsibility and challenging to understand, in order to help patients to better rewrite it.
References
- Spurio MG. ‘Words that Heal’. Psychiatria Danubina. 2015; 27: 21-27. Ref.: https://goo.gl/UA3XKN
- Spurio MG. “Milton Erickson e la Pet therapy”. Quale Psicologia. 2011; 38: 84-88. Ref.: https://goo.gl/HihBzF
- Zeig J. Erickson: Un’introduzione all’uomo e alla sua opera. Astrolabio-Ubaldini. 1990.
- Spurio MG. Il suono della guarigione. Roma. 2015.
- Stroebe M, Shut H. Family matters in bereavement; toward and integrative intra-interpersonal coping model. Psychological Science. 2015; 10: 873-879. Ref.: https://goo.gl/BcXvFe
- American Medical Network Inc. Retrieved on December. 2014.
- Timonen M, Laakso M, Jokelainen J, Ulla Rajala, V Benno Meyer-Rochow, et al. Insulin resistance and depression: cross sectional study. BMJ. 2005; 330: 17-18. Ref.: https://goo.gl/irPSoz
- Yerkes RM, Dodson JD. The relation of strength of stimulus to rapidity of habit-formation. J Comparative Neurology and Psychology. 1908; 18: 459-482. Ref.: https://goo.gl/pQeLT9
- American Institute for Cancer Research. Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective. 2007.
- Paget J. On a Form of Chronic Inflammation of Bones (Osteitis Deformans). Med Chir Trans. 1877; 60: 37-64. Ref.: https://goo.gl/Jw1Qvd
- Spurio MG. The new functional identity: a body that thinks, a mind that feels- frontiers and unexplored territories of the "body and mind zone". Psychiatria Danubina. 2016; 28: 111-115. Ref.: https://goo.gl/ezF3hK