Abstract
Research Article
Identifying mothers experiencing emotional distress in the neonatal intensive care unit. Application of PPTSD questionnaire in a Greek NICU population
Karkani Anastasia*, Theodoraki Martha, Paraskeva Natasa, Kouros Pavlos Aristidis, Pantelis Perdikaris, Rosenblum Ouriel and Mazet Philippe
Published: 07 October, 2022 | Volume 6 - Issue 1 | Pages: 025-031
The birth of a high-risk infant such as an extremely premature infant can represent an important traumatic experience for mothers. Perinatal Post Traumatic Stress Disorder Questionnaire (PPTSDQ) explores retrospectively maternal post-traumatic stress reaction. This shelf-rating questionnaire explores the potential for experiencing posttraumatic symptoms related to childbirth and the ensuing post-natal period. The PTSD questionnaire was originally developed by DeMier and Hynan and their colleagues at the University of Wisconsin and has been widely used in research and in clinical practice for identifying mothers experiencing significant emotional distress during the post-natal period, so they may be referred for mental health services. The present study aims to introduce this tool in perinatal settings as an early intervention. It has been widely used with other measures of post-traumatic stress and depression, such as the Openness Scale from the NEO-PR, the self-report measure of depression BDI-II, the IES (Impact Event Scale) and the EPDS (Edinburgh Postnatal Depression Scale).
Although already a useful clinical instrument the current study used the revised version. This modification refines the response options from dichotomous choices to a Likert scale format by Callahan Borja and Hynan.
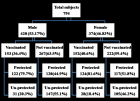
Numerous qualitative and quantitative studies state that premature delivery is a highly stressful event and document the full range of post-traumatic sequelae, such as intrusive recollections, behavioral avoidance, and hyperarousal, as well as attachment difficulties following childbirth. Furthermore, the severity of neonatal complications and gestational age have been found to be predictive of PTSD symptomatology in parents as measured by the PPQ. For this reason, the current study aims to give increased focus to mothers having a premature birth and often expecting their children to die. The sample comprises 25 mothers of prematurely born infants hospitalized in the NICU and 25 mothers of full-term infants born in the maternity ward of the same Greek hospital who responded to the Perinatal PTSD Questionnaire and equally the PERI a postnatal complication rating inventory and the clinical interview for parents CLIP.
Mothers of high-risk infants present post-traumatic stress reactions related to prematurity. The Perinatal PTSD Questionnaire identifies postnatal maternal distress but should not substitute a clinical interview, yet findings indicate that equally identifies pre-existing distress symptoms associated with maternal personality traits that emerged with the traumatic event of the unexpected birth.
Due to the consistency of the population of the experimental group, who come mostly from the provinces, the possibility of a follow- up of the cases is quite limited.
Read Full Article HTML DOI: 10.29328/journal.ida.1001033 Cite this Article Read Full Article PDF
Keywords:
Perinatal stress; Post-traumatic stress disorder; Premature birth
References
- Ballard CG, Stanley AK, Brockington IF. Post-traumatic stress disorder (PTSD) after childbirth. Br J Psychiatry. 1995 Apr;166(4):525-8. doi: 10.1192/bjp.166.4.525. PMID: 7795928.
- Fones C. Posttraumatic stress disorder occurring after painful childbirth. J Nerv Ment Dis. 1996 Mar;184(3):195-6. doi: 10.1097/00005053-199603000-00012. PMID: 8600227.
- McGrath SK, Kennell JH. Doula support: A risk free alternative for pain relief during childbirth." Infant Behavior and Development 21: 566.
- Hodnett ED, Gates S. Continuous support for women during childbirth. The Cochrane Database of Systematic Reviews 2003; CD003766.
- Alexander GR. Preterm Birth: Causes, Consequences, and Prevention, Institute of Medicine (US) Committee on Understanding Premature Birth and Assuring Healthy Outcomes; Behrman RE, Butler AS, editors. Washington (DC): National Academies Press (US); 2007.
- Klauss M, Fanaroff A, Fanaroff J. Care Of the High Risk Neonate. Elsevier Health Sciences, 2013, 6th
- Gennaro S, York R, Brooten D. Anxiety and depression in mothers of low birthweight and very low birthweight infants: birth through 5 months. Issues Compr Pediatr Nurs. 1990 Apr-Jun;13(2):97-109. doi: 10.3109/01460869009009029. PMID: 2272857.
- Mazet Ph. Stoleru S. Premature: risk factor, parental reactions, parent-infant interactions, preventive aspects. In Psychopathology of infants and young children. Paris, Masson. 2003; 3 : 310-319.
- Eliacheff Szejer M. The baby and the ruptures. Separation and exclusion. Editions Albin Michel S.A. 2003 Paris.
- Druon C. Listening to premature babies. Flammarion. 2005.
- Flacking R, Lehtonen L, Thomson G, Axelin A, Ahlqvist S, Moran VH, Ewald U, Dykes F; Separation and Closeness Experiences in the Neonatal Environment (SCENE) group. Closeness and separation in neonatal intensive care. Acta Paediatr. 2012 Oct;101(10):1032-7. doi: 10.1111/j.1651-2227.2012.02787.x. Epub 2012 Aug 2. PMID: 22812674; PMCID: PMC3468719.
- Howe TH, Sheu CF, Wang TN, Hsu YW. Parenting stress in families with very low birth weight preterm infants in early infancy. Res Dev Disabil. 2014 Jul;35(7):1748-56. doi: 10.1016/j.ridd.2014.02.015. Epub 2014 Mar 19. PMID: 24656293.
- KAPLAN DM, MASON EA. Maternal reactions to premature birth viewed as an acute emotional disorder. Am J Orthopsychiatry. 1960 Jul;30:539-52. doi: 10.1111/j.1939-0025.1960.tb02069.x. PMID: 14404378.
- Callahan JL, Borja SE, Hynan MT. Modification of the Perinatal PTSD Questionnaire to enhance clinical utility. J Perinatol. 2006 Sep;26(9):533-9. doi: 10.1038/sj.jp.7211562. Epub 2006 Jul 6. PMID: 16826190.
- Scheiner AP, Sexton ME. Prediction of developmental outcome using a perinatal risk inventory. Pediatrics. 1991 Dec;88(6):1135-43. PMID: 1720234.
- Meyer EC, Zeanah C. Boukydis Z, Lester B. A clinical interview for parents of high-risk infants: concept and applications. Infant Mental Health Journal. 1993. 14.
- Candelori C, Trumello C, Babore A, Keren M, Romanelli R. The experience of premature birth for fathers: the application of the Clinical Interview for Parents of High-Risk Infants (CLIP) to an Italian sample. Front Psychol. 2015 Sep 29;6:1444. doi: 10.3389/fpsyg.2015.01444. PMID: 26483712; PMCID: PMC4586417.
- Pierrehumbert B, Nicole A, Muller-Nix C, Forcada-Guex M, Ansermet F. Parental post-traumatic reactions after premature birth: implications for sleeping and eating problems in the infant. Arch Dis Child Fetal Neonatal Ed. 2003 Sep;88(5):F400-4. doi: 10.1136/fn.88.5.f400. PMID: 12937044; PMCID: PMC1721611.
- Pierrehumbert B, Nicole A, Muller-Nix C. French validation of a post-traumatic stress questionnaire for parents of children at high perinatal risk, Annales Médico-Psychologiques, 2003.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV). Washington DC: Am Psychiatric Association; 1996.
- Quinnell FA, Hynan MT. Convergent and discriminant validity of the perinatal PTSD questionnaire (PPQ): a preliminary study. J Trauma Stress. 1999 Jan;12(1):193-9. doi: 10.1023/A:1024714903950. PMID: 10027153.
- DeMier RL, Hynan MT, Harris HB, Manniello RL. Perinatal stressors as predictors of symptoms of posttraumatic stress in mothers of infants at high risk. J Perinatol. 1996 Jul-Aug;16(4):276-80. PMID: 8866297.
- Ryding EL, Wijma B, Wijma K. Posttraumatic stress reactions after emergency cesarean section. Acta Obstet Gynecol Scand. 1997 Oct;76(9):856-61. doi: 10.3109/00016349709024365. PMID: 9351412.
- Slade P, MacPherson SA, Hume A, Maresh M. Expectations, experiences and satisfaction with labour. Br J Clin Psychol. 1993 Nov;32(4):469-83. doi: 10.1111/j.2044-8260.1993.tb01083.x. PMID: 8298545.
- Korja R, Latva R, Lehtonen L. The effects of preterm birth on mother-infant interaction and attachment during the infant's first two years. Acta Obstet Gynecol Scand. 2012 Feb;91(2):164-73. doi: 10.1111/j.1600-0412.2011.01304.x. PMID: 22007730.
- Fleck P. Connecting Mothers and Infants in the Neonatal Intensive Care Unit. Newborn and Infant Nursing Reviews. 2016; 16: 92-96.
- Rosenblum O, Mazet P, Benony H. Mother and infant affective involvement states and maternal depression, Michigan Association for Infant Mental Health. 1997.
- Vanier C. Premature Birth The Baby, his Doctor and his Psychoanalyst. Ed. Bayard 2013.
- Maman DJ. Why Are You Crying?. editions Odile Jacob, February 2002, Paris.
- Edworthy Z, Chasey R. The role of schema and appraisals in the development of post-traumatic stress symptoms following birth. Journal of Reproductive and Infant Psychology. 2008; 26(2): 123-138.
- Ford E, Ayers S, Bradley R. Exploration of a cognitive model to predict post-traumatic stress symptoms following childbirth. J Anxiety Disord. 2010 Apr;24(3):353-9. doi: 10.1016/j.janxdis.2010.01.008. Epub 2010 Feb 6. PMID: 20176458.
- Zabalia M. For a child psychology in the face of pain. Enfance 2006; 58: 5-19.
- Kloeckner A, Mazet P, De Montgolfier I, Marie P. Later oral disorders in the former premature: description, prevention, JNN Paris. 2006: 126-143.
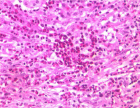
Figures:
Similar Articles
-
Responding to Disasters: More than economic and infrastructure interventionsDavid Crompton OAM*,Ross Young,Jane Shakespeare-Finch,Beverley Raphael AM. Responding to Disasters: More than economic and infrastructure interventions. . 2018 doi: 10.29328/journal.ida.1001007; 2: 014-028
-
Identifying mothers experiencing emotional distress in the neonatal intensive care unit. Application of PPTSD questionnaire in a Greek NICU populationKarkani Anastasia*,Theodoraki Martha,Paraskeva Natasa,Kouros Pavlos Aristidis,Pantelis Perdikaris,Rosenblum Ouriel,Mazet Philippe. Identifying mothers experiencing emotional distress in the neonatal intensive care unit. Application of PPTSD questionnaire in a Greek NICU population. . 2022 doi: 10.29328/journal.ida.1001033; 6: 025-031
Recently Viewed
-
Dual Role of Clinician Managers in Healthcare - Challenges and OpportunitiesAhsana Nazish*. Dual Role of Clinician Managers in Healthcare - Challenges and Opportunities. J Clin Med Exp Images. 2023: doi: 10.29328/journal.jcmei.1001029; 7: 007-013
-
Exceptional cancer responders: A zone-to-goDaniel Gandia,Cecilia Suárez*. Exceptional cancer responders: A zone-to-go. Arch Cancer Sci Ther. 2023: doi: 10.29328/journal.acst.1001033; 7: 001-002
-
The prognostic value of p53 and WT1 expression in cancer: new molecular insights and epigenetics explanations lead to a new medical hypothesisAhed J Alkhatib* and Ilham Ahed Alkhatib. The prognostic value of p53 and WT1 expression in cancer: new molecular insights and epigenetics explanations lead to a new medical hypothesis. Arch Cancer Sci Ther. 2023: doi: 10.29328/journal.acst.1001034; 7: 003-009
-
Anticancer Activity of Genistin: A Short ReviewMd Mizanur Rahaman*, Md Iqbal Sikder, Muhammad Ali Khan and Muhammad Torequl Islam. Anticancer Activity of Genistin: A Short Review. Arch Cancer Sci Ther. 2023: doi: 10.29328/journal.acst.1001035; 7: 010-013
-
Research Progress of BTG2 as a Tumor Prognostic FactorWanting Yang, Peizheng Yang, Yan Li, Yinfeng Yang*, Jinghui Wang*. Research Progress of BTG2 as a Tumor Prognostic Factor. Arch Cancer Sci Ther. 2023: doi: 10.29328/journal.acst.1001036; 7: 014-017
Most Viewed
-
Impact of Latex Sensitization on Asthma and Rhinitis Progression: A Study at Abidjan-Cocody University Hospital - Côte d’Ivoire (Progression of Asthma and Rhinitis related to Latex Sensitization)Dasse Sery Romuald*, KL Siransy, N Koffi, RO Yeboah, EK Nguessan, HA Adou, VP Goran-Kouacou, AU Assi, JY Seri, S Moussa, D Oura, CL Memel, H Koya, E Atoukoula. Impact of Latex Sensitization on Asthma and Rhinitis Progression: A Study at Abidjan-Cocody University Hospital - Côte d’Ivoire (Progression of Asthma and Rhinitis related to Latex Sensitization). Arch Asthma Allergy Immunol. 2024 doi: 10.29328/journal.aaai.1001035; 8: 007-012
-
Causal Link between Human Blood Metabolites and Asthma: An Investigation Using Mendelian RandomizationYong-Qing Zhu, Xiao-Yan Meng, Jing-Hua Yang*. Causal Link between Human Blood Metabolites and Asthma: An Investigation Using Mendelian Randomization. Arch Asthma Allergy Immunol. 2023 doi: 10.29328/journal.aaai.1001032; 7: 012-022
-
An algorithm to safely manage oral food challenge in an office-based setting for children with multiple food allergiesNathalie Cottel,Aïcha Dieme,Véronique Orcel,Yannick Chantran,Mélisande Bourgoin-Heck,Jocelyne Just. An algorithm to safely manage oral food challenge in an office-based setting for children with multiple food allergies. Arch Asthma Allergy Immunol. 2021 doi: 10.29328/journal.aaai.1001027; 5: 030-037
-
Snow white: an allergic girl?Oreste Vittore Brenna*. Snow white: an allergic girl?. Arch Asthma Allergy Immunol. 2022 doi: 10.29328/journal.aaai.1001029; 6: 001-002
-
Cytokine intoxication as a model of cell apoptosis and predict of schizophrenia - like affective disordersElena Viktorovna Drozdova*. Cytokine intoxication as a model of cell apoptosis and predict of schizophrenia - like affective disorders. Arch Asthma Allergy Immunol. 2021 doi: 10.29328/journal.aaai.1001028; 5: 038-040

If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."